- Sustainability
- DE&I
- Pandemic
- Finance
- Legal
- Technology
- Regulatory
- Global
- Pricing
- Strategy
- R&D/Clinical Trials
- Opinion
- Executive Roundtable
- Sales & Marketing
- Executive Profiles
- Leadership
- Market Access
- Patient Engagement
- Supply Chain
- Industry Trends
Johnson & Johnson’s Novel Targeted Oral Peptide Shines in Phase II Trial for Plaque Psoriasis
JNJ-2113, an oral IL-23–receptor antagonist peptide, showed consistency across clinician and patient-reported outcomes in patients with moderate-to-severe plaque psoriasis.
Image credit: fusssergei | stock.adobe.com

Johnson & Johnson’s investigational, oral interleukin (IL)-23–receptor antagonist peptide JNJ-2113 produced promising efficacy compared with placebo in patients with moderate-to-severe plaque psoriasis (PsO) in a Phase IIb trial.1,2 Data from the trial, published in the New England Journal of Medicine (NEJM), show the novel therapy achieved the primary and all secondary endpoints for efficacy in treating the immune-mediated inflammatory condition.
“The science behind advanced treatments for immune-mediated inflammatory diseases like PsO has advanced over the last few decades and patients desire treatment options that combine standard of care efficacy, an acceptable safety profile and flexible routes of administration,” Robert Bissonnette, MD, CEO and Medical Director at Innovaderm Research, said in a press release. “The Phase IIb FRONTIER 1 data, as reported in NEJM, are very encouraging for the ongoing clinical development program and offer a reason to look forward to the continued research of investigational JNJ-2113 as an oral therapy that may offer an attractive and convenient treatment option for patients.”2
Investigators noted that over the past two decades, the treatment of immune-mediated inflammatory diseases has evolved following the approval of several monoclonal antibodies and fusion proteins that act against inflammatory cytokines and their receptors. Because IL-23 has been found to play a critical role in pathogenic T-cell activation in patients with PsO, several biologic therapies that have been approved that target IL-23. Investigators noted that monoclonal antibodies have shown efficacy in modulating the IL-23 pathway, with more favorable safety outcomes compared with older oral therapies, such as cyclosporine, acitretin, methotrexate, and dimethyl fumarate.
“However, biologics have limitations, one of which is that they require intravenous or subcutaneous administration. Many patients prefer oral treatments over injections, and injections are especially problematic among children and among patients with a fear of needles,” the study authors wrote. “In the past 10 years, two oral therapies—apremilast (a phosphodiesterase 4 inhibitor) and deucravacitinib (a tyrosine kinase 2 inhibitor)—were approved for the treatment of psoriasis. However, apremilast has modest efficacy relative to injectable biologics, and data on the long-term safety of tyrosine kinase 2 inhibitors are limited. Thus, there is a need for efficacious targeted therapies that can be administered orally.”1
Investigators of the FRONTIER 1 dose-finding trial randomly assigned 255 patients with moderate-to-severe plaque PsO to receive JNJ-2113 at a dose of 25 mg once daily, 25 mg twice daily, 50 mg once daily, 100 mg once daily, or 100 mg twice daily to compare the different dosing levels with a placebo over 16 weeks. The trial’s primary endpoint was a reduction of at least 75% from baseline in the Psoriasis Area and Severity Index (PASI) score at week 16.
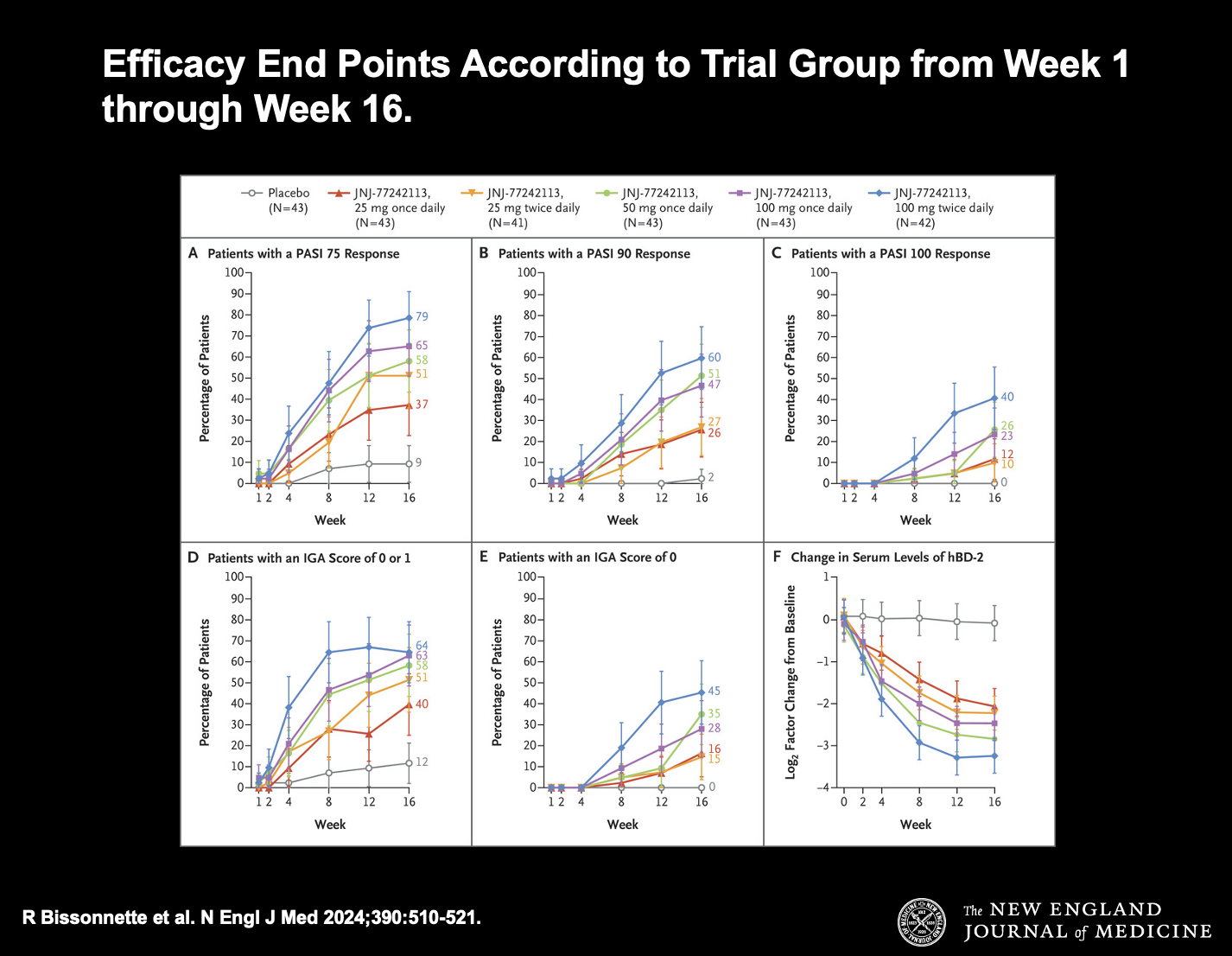
Figure 1. Efficacy End Points According to Trial Group from Week 1 through Week 16.
Scores on the Psoriasis Area and Severity Index (PASI) range from 0 to 72, with higher scores indicating greater extent or severity of psoriasis. PASI 75 response, PASI 90 response, and PASI 100 response refer to reductions from baseline of at least 75%, 90%, and 100%, respectively, in the PASI score. Scores on the Investigator’s Global Assessment (IGA) range from 0 (clear skin) to 4 (severe disease); a score of 1 indicates minimal disease. 𝙸 bars denote 95% confidence intervals. For serum levels of human β-defensin 2 (hBD-2), 𝙸 bars indicate linear mixed-effect model–based 95% confidence intervals. The widths of the confidence intervals have not been adjusted for multiplicity and should not be used to infer definitive effects of JNJ-77242113 for the secondary end points.
CREDIT: New England Journal of Medicine
Secondary endpoints included an IGA score of 0—indicating clear skin—or 1—indicating minimal disease—at week 16; decrease from baseline of at least 90% in the PASI score at week 16; decrease from baseline of 100% in the PASI score at week 16; PASI score change from baseline at week 16; and change from baseline in BSA involvement at week 16.
Among patients enrolled in the trial, the mean PASI score at baseline was 19.1, the mean duration of PsO was 18.2 years, and 78% were previously administered systemic therapy.
At week 16, a greater percentage of patients administered JNJ-2113 achieved a PASI 75 response compared with placebo. Among the treatment groups, PASI 75 was achieved by 37% of patients in the 25-mg once-daily cohort, 51% in the 25-mg twice-daily cohort, 58% in the 50-mg once-daily cohort, 65% in the 100-mg once-daily cohort, and 79% in the 100-mg twice-daily cohort compared with 9% in the placebo cohort. Findings for the secondary endpoints and patient-reported outcomes were generally consistent with data for the primary endpoint, according to the study.
The most common adverse events (AEs) observed in the trial included COVID-19, which was reported in 12% of patients in the placebo cohort and 11% of patients across the various JNJ-2113 dosing cohorts, and nasopharyngitis, which was observed in 5% of patients in the placebo cohort and 7% of patients in the JNJ-2113 cohort. Investigators did not find evidence of increases in AEs related to higher doses of the novel therapy.
“[JNJ-2113], an oral [IL]-23–receptor antagonist peptide, showed a dose–response relationship and greater efficacy than placebo, as measured by the PASI 75 response at week 16, in patients with moderate-to-severe plaque psoriasis. Overall, there was no evidence of a relationship between the [JNJ-2113] dose and the incidence of [AEs],” the study authors concluded.1
The investigators added that the findings from the trial indicate the experimental therapy has the potential to treat a range of additional IL-23-mediated diseases. As a result, Johnson & Johnson has initiated the Phase IIb ANTHEM-UC trial, which will analyze the safety and efficacy of JNJ-2113 vs. placebo in patients with moderately to severely active ulcerative colitis.
“The impacts of living with moderate-to-severe plaque PsO are felt across all aspects of life and many patients do not seek advanced treatments because they have concerns with injectables and prefer an oral therapeutic option,” Lloyd Miller, MD, PhD, vice president, Immunodermatology disease area leader, Johnson & Johnson, said in the release. “We are encouraged by the study findings published in NEJM, including consistency across clinician and patient-reported outcomes and objective biomarkers. If approved, JNJ-2113 has the potential to improve both clinical and quality of life outcomes.”2
References
1. Bissonnette R, et al. An oral interleukin-23–receptor antagonist peptide for plaque psoriasis. N Engl J Med. 2024;390:510-21. DOI: 10.1056/NEJMoa2308713.
2. Investigational targeted oral peptide JNJ-2113 demonstrated positive results in moderate-to-severe plaque psoriasis in Phase 2b study published in New England Journal of Medicine. Johnson & Johnson. News release. February 7, 2024. Accessed February 8, 2024. https://www.jnj.com/media-center/press-releases/investigational-targeted-oral-peptide-jnj-2113-demonstrated-positive-results-in-moderate-to-severe-plaque-psoriasis-in-phase-2b-study-published-in-new-england-journal-of-medicine
Cell and Gene Therapy Check-in 2024
January 18th 2024Fran Gregory, VP of Emerging Therapies, Cardinal Health discusses her career, how both CAR-T therapies and personalization have been gaining momentum and what kind of progress we expect to see from them, some of the biggest hurdles facing their section of the industry, the importance of patient advocacy and so much more.
