Discovering the Need for Vaccines Against RNA Viruses: Q&A with Thomas Rademacher, MD, PhD
Rademacher discusses his early work with trying to develop a vaccine for Ebola.
Thomas Rademacher is considered by some to be one of the founders of biotech. Most recently, he co-founded and serves as CEO of Emergex, which works on developing new types of vaccines. In this first part of Pharmaceutical Executive’s conversation with him, he discusses how he got into vaccine development.
Pharmaceutical Executive: How did you get involved with Emergex?
Thomas Rademacher: We founded the company under unusual circumstances, as I was near retirement. At the time I was at the College of London as professor emeritus. It was about 2014 and there was the Ebola outbreak. Everyone went into a miniature panic, as it was the first eye-opener to these viruses that can come in and spread quickly. There wasn’t really anything else around, and this was one of those illnesses where there were immediate issues. I think the UK only had one or two containment facilities.
There was a great worry about that, so I got called in. I was asked if I had a blank slate and all of the money in the world, how would I come up with something quickly in case this Ebola thing becomes highly transmissible and starts spreading.
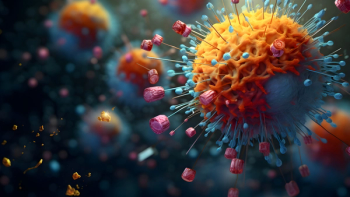
I had been an immunologist but not a virologist, so I had to dive deep into that. What I found is that Ebola is an RNA virus, which I knew little about. Then I discovered that these viruses exist as clouds. There’s not one of them, there’s a population that works together. It was fascinating to me that victims were being attacked by a cloud of viruses that were all slightly different. They’re all very small and don’t carry enough information in an individual virus, so they need to work together.
A DNA virus contains 100s of genes and all of the information to do what it needs to do. So, here you have RNA viruses that function as clouds. Then we realized that Polio is an RNA virus, and so is yellow fever and COVID-19. All of the world’s nasties are RNA.
PE: Where did you go from there?
Rademacher: Then we asked how we could go after these, which meant we had to ask how did our great medical establishment learn to deal with clouds of viruses. At that point, they hadn’t. The only ways to deal with RNA viruses were live, attenuated vaccines. Everything else had been a failure.
The challenge was to discover what makes a live, attenuated vaccine work. How can you attack a cloud of viruses? I always say that there was no Wuhan strain of SARS COVID 2. It’s simply a mathematical sum of all of the individuals. When it became omicron, the frequency of all of these guys changed. It was the same cloud, but with a different ranking among the individual viruses.
I came across a paper that said if you got bit four times by a mosquito carrying dengue fever, you got four different inoculums. When you transmit the cloud, you only transmit one or two members of the cloud, which then have to reform the cloud. That’s where mathematics comes in. How do you take one member of a cloud, put it into somebody, and have it remake the cloud? It’s a fascinating issue.
The issue here is that no one is going to make live, attenuated vaccines anymore. These things were done back in the 20’s, 40’s, and the 60’s. These days, you can’t go to regulators and say that you have a live, attenuated Ebola vaccine that you’d like to test. They’d ask if it would give the test subjects Ebola, and the answer would be that you don’t know that it won’t.
PE: If you can’t really go after live attenuated vaccines, how can you do it synthetically?
Rademacher: That got to another problem. If I take a yellow fever vaccine, that’s a live yellow fever virus. If I do anything to it at all that causes it to die, then it doesn’t work. You can inject somebody with dead yellow fever vaccine and it doesn’t work, and you can give somebody live yellow fever vaccine and it does work. The body recognizes life, but the question is how does it recognize life in a virus?
The challenge became discovering what was in these viruses that made the body think they were alive. I found it fascinating from a mathematics point of view, and from the point of view of determining what’s more important: the virus or the viral infected cell. When the cell gets infected, does it become the virus?
The body deals with it by killing the viral infected cell, which is how live, attenuated vaccines work. They generate an immune response against the viral infected cell, but the body doesn’t seem to care about the actual virus at all, just the cell. It can’t recognize the virus, but it can recognize infected cells.
A couple of the big pharmas spent a vast sum of money on developing a vaccine for Ebola. By the time they got ready to test, Ebola had gone away. The issued that evolved out of that in 2014 and 2015 was the issue of preparedness. This meant that, generally speaking, we needed to have vaccines ready before the outbreak because you can only test it at the time of the outbreak.
So, pharma had to figure out if it was worth it to spend money on developing a vaccine it couldn’t test and could possibly just sit in a freezer somewhere.
Our challenge was to determine if we could trick the body into reacting to a dead virus as if it was a live virus. We also had to figure out if it could be made safely and affordably, and if it could be distributed any country it needed to go.
Newsletter
Lead with insight with the Pharmaceutical Executive newsletter, featuring strategic analysis, leadership trends, and market intelligence for biopharma decision-makers.